What are the key differences between private and NHS menopause care in the UK?
Private menopause care usually involves longer consultation times, faster appointment availability, and access to more comprehensive hormone testing. NHS care follows National Institute for Health and Care Excellence (NICE) guidelines and is free at the point of use, but is often limited by appointment length and treatment scope. Private clinics like Future Care Medical offer access to British Menopause Society (BMS) accredited practitioners, tailored hormone replacement therapy (HRT), and private laboratory tests, including full endocrine panels. Your choice depends on how complex your symptoms are, how quickly you need support, and what your budget allows.
Here's What We Have Covered In This Article
Frustrated with Your Menopause Care? You’re Not Alone
Many women feel dismissed during NHS appointments when discussing menopause symptoms. Some are told they’re too young or just stressed, which can delay diagnosis and leave symptoms untreated.
Online platforms like Mumsnet and Reddit are full of real accounts from women who later discovered they were in perimenopause. These stories often lead to exploring private menopause support, where appointments allow time for full discussion and more proactive care. For many, this shift helps improve emotional wellbeing, reduce health anxiety, and restore confidence during a time of hormonal change.
Pro Tip: Keep a digital symptom diary to track your progress and streamline GP appointments.
Book a Private Menopause Consultation
Speak to a GP who specialises in menopause care. Get clear answers, fast.
What Support Does the NHS Offer for Menopause?
NHS GPs follow NICE guidelines recommending symptom-based diagnosis for women over 45. Support may include basic HRT (oestradiol and progestogen), lifestyle advice, and referrals to specialists if symptoms are complex.
Appointments are usually limited to ten minutes. Blood testing is not routinely offered unless early menopause is suspected. Body-identical or compounded HRT is rarely available through NHS services. While NHS menopause clinics do exist, waiting times can be several months.
What Can You Expect from a Private GP for Menopause Support?
Private menopause appointments typically last 30 to 60 minutes and provide a more in-depth review. These may include:
- Hormone testing for oestradiol, FSH, luteinising hormone, testosterone, and thyroid function
- Digital tools for symptom tracking
- Tailored HRT plans including testosterone, body-identical or plant-based treatments
- Nutritional and lifestyle guidance
Clinics like Future Care Medical offer 30-minute menopause consultations priced at £295. This includes a detailed treatment plan. Laboratory tests and prescriptions are additional. The service is led by clinicians trained under British Menopause Society standards.
Private care often includes a full hormone profile review, using lab-based hormone testing and symptom scoring tools. Patients receive written plans that help track changes over time, offering clarity in diagnosis and boosting treatment confidence.
HRT, Tests and Follow Ups How Do NHS and Private Care Compare?
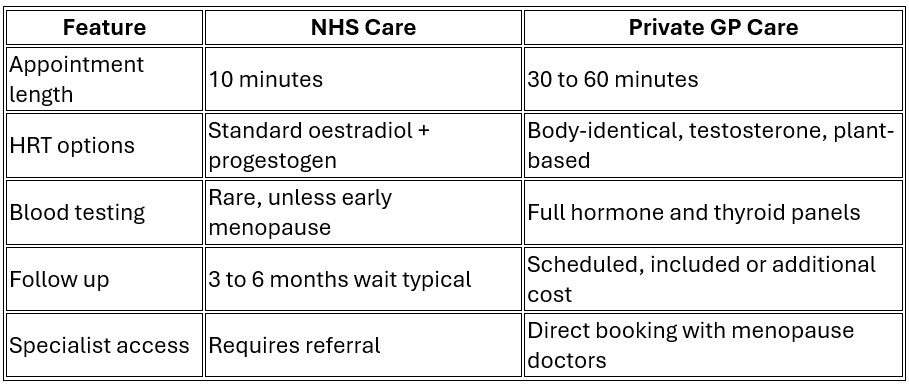
NHS care remains valuable for those with mild, stable symptoms. Private clinics offer direct access care with shorter wait times, patient-led follow ups, and broader prescribing flexibility.
Pro Tip: Always ask whether follow ups and test fees are included before booking privately.
Is It Worth Paying for a Private GP to Manage Your Menopause?
Women who opt for private care often do so after feeling their NHS experience lacked depth or pace. A typical private consultation offers faster access and access to more prescribing options.
Future Care Medical charges £295 for a 30-minute consultation. This includes a tailored plan following discussion and history taking. Prescriptions and tests are charged separately. If NHS care has been slow, or symptoms are complex, private clinics may offer a more responsive and personalised experience.
Patients often report quality of life improvements from private care. Faster access, deeper hormone insight, and ongoing monitoring help them regain energy, sleep, and emotional stability.
When NHS Menopause Care Might Be Enough
Some women find NHS care works well, particularly when:
- Symptoms are manageable or improving
- Their GP is informed and supportive
- They’re already on standard HRT and need occasional reviews
Tools like the Balance App or Patient Access can complement NHS care by tracking symptoms and improving communication during appointments. These digital symptom trackers can enhance shared decision making and promote patient empowerment.
When Private Care Could Be the Better Choice
Why is testosterone considered in menopause care?
Testosterone supports libido, cognitive function, and energy. While women produce it in smaller amounts, levels often decline during menopause.
The NHS rarely prescribes testosterone unless under specialist care. Private GPs can prescribe it when symptoms and lab results support the need. It’s usually given as a gel, monitored with blood tests, and dosed carefully to match female hormone levels.
While not all women require it, those who do often report significant symptom improvement when it’s introduced under proper guidance.
Private menopause care may be more appropriate if:
- You experience ongoing symptoms despite NHS support
- You’ve been refused treatment options such as testosterone
- You want test results and answers within days rather than weeks
- You prefer working with menopause specialists directly
Clinics may also use digital menopause diaries, symptom scoring apps, and offer integrated care models including virtual menopause consultations.
Get a Full Hormone Profile Today
Advanced blood testing to understand your symptoms and start personalised care.












